
Payer Strategy

What is Payer Intelligence?
Payer Intelligence is a cutting-edge tool designed to facilitate a deep understanding of the coverage and access landscape orchestrated by payers.
This dynamic platform offers an intuitive and user-friendly interface that grants you the ability to analyze the ebb and flow of lives covered by payers for diverse products across various indications.
The tool leverages data from MMIT to provide policy coverage insights and enrollment information, enabling you to seamlessly track month-over-month shifts in coverage, enrollment, and claims patterns.
It combines medical and pharmacy claims with payer/plan formulary coverage, and can also include total cost of care from John Hopkins.
The Challenges

How would Payers react?
- Communicating value-based competitive advantage of the drug to payers based on RWE (Real-World Evidence)
- Providing compelling communication to payers

What is the competitive landscape?
- Analyze which of the payer contracts are working and which ones are not
- Deep dive into plans where competition has advantageous position over our product

How to effectively communicate?
- Providing compelling communication to Providers

How to accelerate the growth of the brand Fine-tune the strategy?
- Discovering key drivers to accelerate the growth of the brand
- Determining the top drivers for rejection and the tactics that can be used to minimize the rejection
Why Payer Intelligence?
Smarter insights to empower payer engagement

Analyzes payer landscapes and competitors to gain a competitive advantage for your product

Utilizes state-of-the-art analytical techniques to accelerate decision-making in competitive contracting scenarios

Educates physicians and providers about unmet needs as a way to remove perceived access barriers

Ensures access journey needs are met throughout the life sciences product lifecycle

Better positioning of your product VS competition with value based pricing
Benefits
Payer Intelligence brings forth a multitude of benefits that empower your organization’s strategic planning and execution
Early Anomaly Detection
Identify data anomalies before embarking on in-depth coverage analysis, ensuring the accuracy and reliability of your insights.

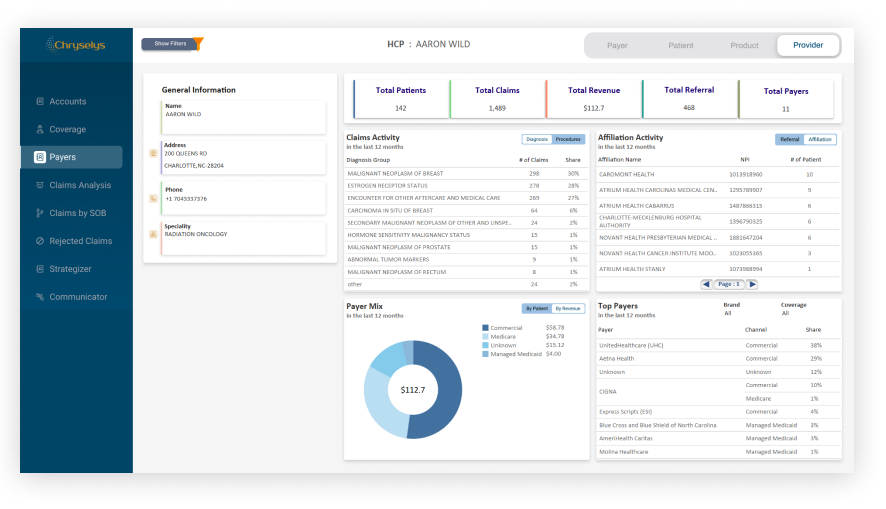
Comprehensive Payer Landscape
Gain a holistic view of the payer landscape, enabling you to make well-informed decisions about your payer access strategy.

Competitor Insights
Understand how your brand stacks up against competitors in terms of claims volume, coverage status, and payer mix, allowing you to refine your approach.

Enhanced Claims Analysis
Leverage claims data to enhance your understanding of payer and claims landscapes.
Unique Selling Points


What sets our Payer Intelligence Tool apart

Granular Insights
Unparalleled insights into claims volume, payer coverage status, and lives shift on regional and national scales.

Holistic Claims and Payer Mix Analysis
Offers a comprehensive view of claims and payer mix for both competitor brands and your own, facilitating strategic comparisons to enhance your competitive edge.

The Payer Intelligence Tool simplifies complexity, illuminates trends, and empowers you to chart a course of action grounded in data-driven insights.
Welcome to a new era of payer intelligence – where your journey towards informed, effective payer strategies begins here.
We Have More to Offer


Accelerate trial recruitment by partnering with key physicians investigators and finding the right patients.


Avail a repository of ready-to-use patient data to solve complex business challenges. Visualize all your data in one place.
For inquiries contact us today.
Where innovation meets expertise, and excellence is the only outcome.







