Market Access today is more than just securing formulary status, it’s about navigating a complex, evolving ecosystem of payers, patients, providers, and policies. Chryselys’ Market Access Intelligence delivers a comprehensive, AI-powered approach to decoding access challenges, optimizing contracts, and enabling confident prescribing decisions.
Built for real-world market complexity, our solution blends structured datasets (claims, rebates, access metrics) with unstructured sources (payer policy PDFs, formulary docs, coverage restrictions) to provide a 360° view of the access landscape.
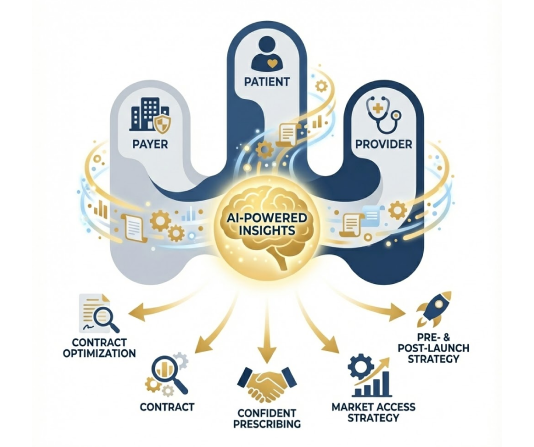
Market Access Intelligence by Chryselys combines deep domain expertise, AI-powered automation, and “white-glove” stewardship to deliver more than just data, it delivers action-ready insights. From pre-launch strategies to post-launch optimization, we help pharma companies bridge access gaps with clarity and confidence.

Pinpoint restrictions like PA, ST, NDC rejections, and plan-level exclusions

Align IQVIA, MMIT, HUB data through a robust payer MDM layer

Forecast leakage, model scenarios, and refine contract performance

Map competitor access shifts and coverage trends

Support field teams and HCPs with accurate, real-time coverage clarity

Identify root causes and reduce abandonment






Our unified solution synthesizes multiple datasets and stakeholder needs into a single, analytics-ready intelligence layer.

Combines claims, coverage documents, formulary data, and PDFs into one cohesive intelligence layer.

Crosswalks IQVIA ↔ MMIT ↔ SP/HUB, resolving inconsistencies with GenAI + human stewardship.

Our AI models are backed by rigorous manual validation for accuracy and refinement.

Extracts policy nuances, flags anomalies, and generates research summaries—at scale.

Supports Oncology, Immunology, CNS, Rare, CV/Metabolic, and more.
Market Access Intelligence is tailored for teams navigating high-stakes access decisions:

Formulary access, contract strategy, G2N analytics, IRA forecasting

Launch readiness, competitive intelligence, field planning

Denial analytics, copay program optimization, patient journey mapping

Payer policy extraction, evidence generation, coverage impact modeling

Unified payer data management and analytics-ready datasets
Let Chryselys help you connect the dots across payers, plans, and patient journeys with clarity, speed, and confidence.